Let's be direct: managing patients with chronic conditions is a constant challenge. You see them for 15 minutes in the office, but their health is determined by what happens in the days and weeks between visits. Remote patient monitoring (RPM) bridges that gap, giving you the daily insights needed to provide proactive care. The challenge isn't deciding if RPM is valuable; it's choosing from the crowded field of RPM companies. Each one has a different technology platform, service model, and pricing structure. Some focus narrowly on devices or data platforms, while others deliver a true end-to-end service. Among today’s leading RPM companies, a small subset—including 1bios—combine advanced AI technology, U.S.-based care teams, and compliance-first processes that ensure consistent reimbursement and lasting results.
This guide is designed to make that choice easier by providing a side-by-side look at the industry's top players, so you can find a solution that works for your patients, your staff, and your bottom line.
Key takeaways
- Partner for service, not just software: The most successful RPM programs are run by full-service partners who manage everything from patient enrollment and device logistics to clinical monitoring and billing, freeing your staff to focus on in-office care.
- Prioritize simplicity and integration: Your RPM solution should make life easier for everyone. Look for easy-to-use cellular devices for patients and a platform that integrates seamlessly with your EMR to ensure high adoption rates and a smooth workflow for your team.
- Plan your launch to ensure a strong ROI: A successful RPM program requires a clear strategy for implementation. By defining your goals, training your staff, and creating a patient enrollment plan, you can overcome common challenges and build a sustainable new revenue stream.
What is Remote Patient Monitoring (RPM)?
At its core, Remote Patient Monitoring (RPM) is a way for you to care for your patients even when they aren’t in your office. It uses digital technology to collect health data from patients in their homes—like blood pressure, weight, or blood sugar levels—and securely transmits it to you and your care team. This steady stream of information gives you a much clearer picture of a patient's health between visits, allowing you to spot potential issues before they become serious problems.
For practices managing patients with chronic conditions like hypertension, heart failure, or diabetes, RPM is a game-changer. It moves care from being reactive to proactive. Instead of waiting for a patient to report symptoms, you can see the data in near real-time, make timely adjustments to their care plan, and provide support when they need it most. It’s about creating a stronger connection with your patients and empowering them to take a more active role in managing their own health, all while creating a new, sustainable revenue stream for your practice.
How RPM technology works and its benefits
The process is straightforward. Your patient uses a simple, cellular-enabled medical device at home—think a blood pressure cuff, scale, or glucometer. The device automatically captures a reading and sends the data to a secure platform for your team to review. There’s no need for the patient to have a smartphone or Wi-Fi, which removes a major barrier for many, especially older adults.
The benefits are clear for everyone involved. Patients feel more connected and supported, knowing their health is being monitored daily. This consistent oversight often leads to better health outcomes and fewer hospitalizations. For your practice, RPM provides the data you need to make more informed clinical decisions, helps you manage your patient population more efficiently, and opens up significant new revenue opportunities through established CPT codes for remote care.
Just as importantly, the right RPM company will make compliance and documentation effortless. Every interaction, data point, and patient touchpoint should be automatically logged and audit-ready, ensuring you capture every eligible reimbursement without risk.
The core parts of an RPM system
A successful RPM program has three main components working together. First are the devices themselves. These need to be reliable, easy for patients to use right out of the box, and automatically transmit data without any complicated setup.
Second is the software platform. This is the central hub where all patient data is organized and presented in a clear, actionable way. A good platform will integrate smoothly with your existing Electronic Medical Record (EMR) system to avoid creating extra work for your staff. Ideally, it will automatically send relevant data to a practice's existing billing platform.
Finally, and most importantly, is the clinical team that monitors the data and engages with patients. This team acts as an extension of your practice, reviewing daily readings, identifying trends, and reaching out to patients to provide coaching and support when needed.
Many practices turn to third-party RPM companies to handle one or all of these key areas. This is recommended, as it helps reduce the risk and complexity of handling these programs DIY. Still, even within in this field, offerings differ greatly (as will be explored below), ranging from a simple platform to a comprehensive turnkey RPM service.
How RPM improves patient care and revenue
RPM directly translates to better, more proactive patient care. When the team sees a patient's blood pressure trending upward, you can intervene with a medication adjustment or a telehealth call before it leads to an emergency room visit. This consistent engagement also helps patients understand their condition better and stick to their treatment plans. It’s a powerful tool for improving outcomes and reducing hospital readmissions.
From a business perspective, RPM creates a reliable, recurring revenue stream. Medicare and many private insurance plans reimburse for these services, including the initial device setup and ongoing monitoring. By offering a Chronic Care Management (CCM) program powered by RPM, you can significantly increase practice revenue while offloading the day-to-day monitoring work to a trusted partner, freeing up your staff to focus on in-office care.
But not all RPM companies handle billing and compliance the same way. Without built-in documentation and RCM expertise, many practices struggle to capture the full value of their work or risk failing payer audits. Look for a company that takes a compliance-first approach—automatically tracking every reading, note, and communication so billing is always accurate, complete, and audit-ready.
BLOG: Why Most RPM Programs Fail at Enrollment (and How to Fix It)
Comparing the top RPM companies
Choosing an RPM partner is a big decision for your practice. The right company can feel like an extension of your team, helping you improve patient outcomes and generate new revenue without adding to your staff's workload. The wrong one, however, can create more headaches than it solves, leading to frustrated staff and disengaged patients. The market is full of options, and each company offers a slightly different approach. You'll find full-service turnkey solutions that handle everything from patient onboarding to billing, as well as tech-only platforms that give your team the tools to run the program yourselves.
To help you find the right fit, it’s important to understand this landscape. Some vendors focus on specific chronic conditions like hypertension or diabetes, while others offer a broader platform for various patient needs. Some provide the clinical staff to manage daily monitoring and patient interactions, and others expect your team to handle those responsibilities.
Below is a look at some of the top players in the RPM space and what makes each one unique. As you review these RPM companies, pay attention to how each handles the three pillars of a successful program: patient enrollment, service delivery, and billing. Only a few, like 1bios, deliver all three with their own in-house technology, clinical staff, and compliance infrastructure—ensuring end-to-end reliability rather than fragmented execution.
1bios
1bios is a turnkey RPM service built specifically for small to mid-size practices that want a true partner, not just a software platform. The company combines its AI-powered technology with an in-house clinical team to manage every part of an RPM program from start to finish. This includes patient enrollment, device setup, daily monitoring, and insurance billing. By taking on these operational tasks, 1bios helps practices generate recurring revenue and improve patient care without overburdening staff.
The company’s focus is on making RPM simple, compliant, and effective. Every component of the 1bios model—from AI-driven eligibility scans and outreach to U.S.-based clinical monitoring and billing support—is handled entirely in-house. With thousands of providers and more than 100,000 patients served through its RPM and CCM programs, 1bios has built a strong reputation for quality, compliance, and measurable financial and clinical results—with zero compliance failures to date.
HealthSnap
HealthSnap is a virtual care management platform that uses cellular-enabled devices, which is a great feature for patients who may not have a smartphone or reliable Wi-Fi. HealthSnap's system is designed to deliver continuous care by providing your team with real-time patient data and alerts, helping you stay connected with patients between visits. This allows for timely interventions when a patient's readings are outside of their normal range. While its cellular-enabled devices are convenient, smaller practices may find its one-size-fits-all model expensive and complex to customize.
Optimize Health
Optimize Health delivers a flexible, user-friendly platform but expects your staff to handle most of the outreach, monitoring, and billing. That means practices without extra administrative capacity may struggle to keep enrollment and compliance documentation consistent. Optimize a strong fit for organizations with dedicated RPM staff, but less so for clinics seeking a fully managed partner.
Cadence Care
Cadence focuses narrowly on cardiometabolic conditions like hypertension and heart failure and provides its own remote care teams. However, Cadence's model is typically structured around large enterprise partnerships, making it less adaptable for independent or multi-specialty clinics. The limited condition coverage can also restrict long-term program growth across a broader patient base.
Athelas
Athelas emphasizes quick setup and easy connectivity, helping practices launch RPM programs fast. But Atheleas' technology-first model relies heavily on automated alerts and offshore support staff rather than U.S.-based care teams. That can make it harder for smaller practices to maintain the personalized patient relationships and compliance documentation auditors expect.
Health Recovery Solutions
HRS offers a wide array of telehealth and RPM tools designed for hospitals and post-acute care networks. Its depth and scalability are impressive, but the platform can be overbuilt for independent clinics that need simplicity and close partnership rather than enterprise-grade infrastructure. Many smaller practices find it resource-intensive to implement and manage.
Accuhealth
Accuhealth (now part of TelliHealth) is known for its connected devices and 24/7 vitals monitoring. However, much of its service delivery depends on third-party integrations and off-the-shelf hardware, which can create data inconsistencies and device replacement issues. Accuhealth compliance and documentation workflows also require close oversight by your billing team.
TimeDoc Health
TimeDoc Health combines RPM and CCM tools and integrates with most EHRs. While TimeDoc supports multiple care-management programs, practices are typically responsible for their own staffing and patient engagement. Without embedded enrollment or billing support, many smaller teams struggle to scale beyond a small patient subset.
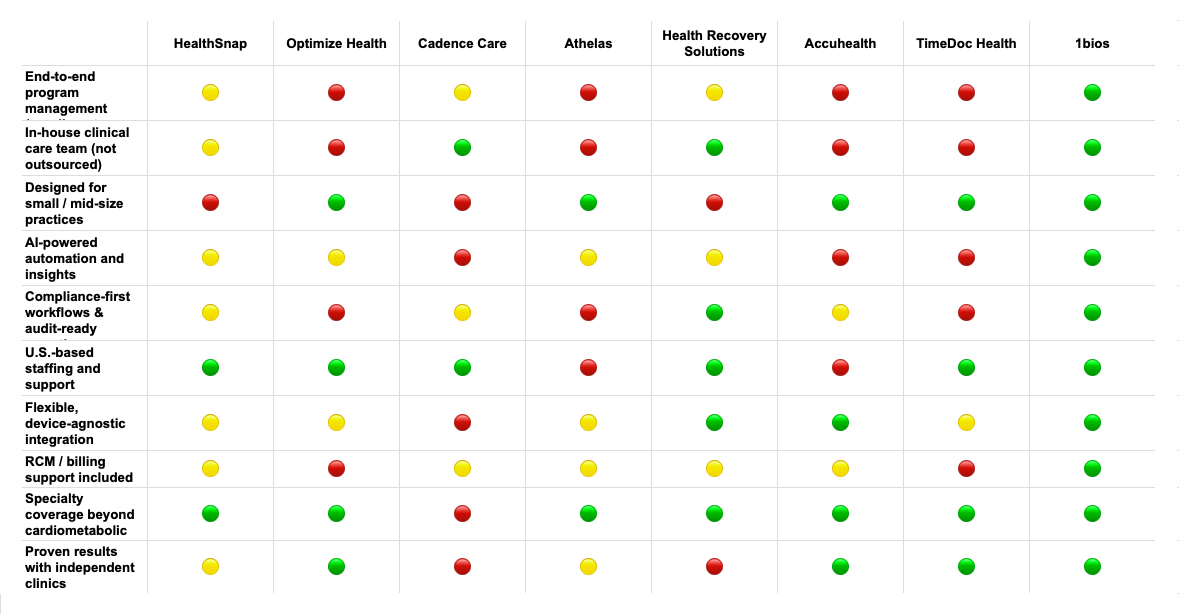
🟢 = Fully supported / best-in-class
🟡 = Partial or limited support
🔴 = Requires significant effort from your team
Across all these options, 1bios stands apart because it combines the simplicity of a fully managed program with the safety and precision of a compliance-first partner. While other companies may require your staff to handle enrollment, monitoring, or billing—or outsource key work overseas—1bios keeps everything under one U.S.-based roof. Our AI-powered technology, in-house care team, and proven processes ensure your program runs smoothly from start to finish: patients stay engaged, your staff stays focused on in-clinic care, and you get paid correctly every time. For practices that want results without extra workload or risk, 1bios is the clear choice.
Key features to look for in an RPM solution
Choosing an RPM partner is a big decision, and not all solutions are created equal. As you compare your options, it’s helpful to look past the sales pitch and focus on the specific features that will make a real difference for your practice and your patients. Here are the key capabilities to look for to ensure your RPM program is successful, sustainable, and simple to manage.
1. Flexible device options and management
Your patients aren’t all the same, and their monitoring devices shouldn’t be either. A great RPM partner offers a range of high-quality, cellular-enabled devices—like blood pressure cuffs, scales, and glucometers—that are easy for patients to use right out of the box. Look for a company that handles all the logistics for you, from shipping devices directly to patients to providing clear setup instructions. The best solutions also include resources like teach-back videos and patient support, so your staff isn’t stuck playing tech support.
2. Clear data and actionable reports
A flood of patient data is useless without a way to make sense of it. Your RPM platform should do the heavy lifting, turning raw numbers into clear, actionable insights. Instead of just showing a list of readings, the system should highlight trends, flag abnormal results, and present the information in an intuitive dashboard. This allows your clinical team to see at a glance which patients need immediate attention, so you can intervene proactively without spending hours digging through data. The goal is to make informed decisions, faster.
3. Tools to keep patients engaged
An RPM program only works if patients consistently use their devices. That’s why patient engagement tools are so important. Your RPM partner should provide features that help patients stay on track, like automated text reminders to take their readings and educational content to help them understand their condition. Some platforms also offer two-way messaging, which gives patients a simple way to connect with their care team. These tools empower patients to take an active role in their care, leading to better adherence and improved health outcomes.
4. Support for your clinical decisions
The right RPM partner acts as an extension of your team, not just a software provider. Look for a company that offers clinical monitoring services staffed by trained professionals. This team can watch for critical alerts, follow up with patients, and escalate issues to your providers when necessary. This kind of support is a game-changer for smaller practices, as it helps you manage a larger patient panel without overwhelming your in-house staff. It ensures your patients get timely attention while freeing your team to focus on in-office care.
It’s also worth asking whether your RPM partner uses AI to enhance these workflows. Platforms like 1bios embed AI tools that automatically flag high-risk patients, summarize documentation for billing, and generate compliance-ready reports. This not only reduces administrative time but also helps maintain consistent quality and audit readiness as your program scales.
5. Simplified billing and revenue management
Let’s be honest: RPM billing can be complicated. The CPT codes have specific requirements for time and data transmission that can be tricky to track. A top-tier RPM solution will have billing built right in. It should automatically log the time spent on patient care and generate the documentation you need for every claim. This not only ensures you’re capturing all the revenue you’ve earned but also prepares you to pass any payer audit with confidence. This makes the financial side of RPM financially sustainable for your practice.
6. Seamless EMR and system integration
If an RPM platform doesn’t integrate with your existing EMR system, it’s creating more work, not less. Manual data entry is a recipe for errors and wasted time. Look for a solution that offers seamless, bidirectional integration with your EMR. This means patient data from monitoring devices flows directly into their chart, and any notes your team makes are synced automatically. When your platforms can share information, your staff has a complete, up-to-date view of each patient without having to jump between different systems.
7. Top-notch security and compliance
Protecting patient health information is your top priority, and it should be your RPM partner’s, too. Any solution you consider must be fully HIPAA-compliant, with robust security measures to safeguard sensitive data. Ask potential vendors about their security protocols, such as how they ensure all data transmitted from RPM devices is encrypted and stored securely. A trustworthy partner will be transparent about how they protect patient information and help you meet all your compliance obligations. This isn't just about following the rules—it's about maintaining the trust you've built with your patients.
Breaking down RPM costs and ROI
When you’re considering any new service for your practice, the first question is usually about the bottom line. Let's be direct: implementing a RPM program involves an investment. But it’s crucial to see it as just that—an investment, not just an expense. The costs are balanced by significant returns, both in new revenue and in operational improvements that make your practice run more smoothly.
Understanding the full financial picture helps you see how RPM can be a profitable and sustainable part of your practice. The costs typically fall into three main categories: initial setup fees, ongoing monthly service fees, and the cost of the devices themselves. On the other side of the ledger, you have a powerful new revenue stream from billing for RPM services and major gains in efficiency that save your staff time and reduce burnout. Let’s break down each of these components so you can see how the numbers really work.
Setup and implementation fees
Getting your RPM program off the ground involves some initial, one-time costs. Think of this as the foundation for your program. These fees typically cover the technical setup, which includes integrating the RPM software with your existing EMR system. A smooth integration is non-negotiable, as it ensures patient data flows seamlessly and securely. This fee also usually covers initial training for you and your staff, so everyone feels confident using the new platform from day one. The best RPM partners make this process feel effortless, handling the technical heavy lifting so you can stay focused on your patients.
Monthly service fees
Once you're up and running, you’ll have a recurring monthly service fee. This fee is the engine that keeps your RPM program going. It generally covers your license to use the software platform, secure data hosting, and ongoing technical support for your team. Depending on the partner you choose, this fee might also include clinical monitoring services, where their team of nurses helps watch over patient data and alerts you to any readings that need your attention. Pricing models vary, but they are often structured on a per-patient, per-month basis. This allows you to scale your program as you enroll more patients, and the fees are designed to be covered by insurance reimbursements, making the program financially sustainable.
Device costs
Of course, you can’t have remote monitoring without the monitoring devices. This cost covers the physical hardware your patients will use at home, like blood pressure cuffs, weight scales, and glucometers. Some RPM companies require you to purchase and manage this inventory yourself, while others offer leasing options or include the devices as part of their service package. The best approach for most small to mid-size practices is to work with a partner who handles all the device logistics—from shipping devices directly to patients to providing tech support and replacements. This frees you from becoming a medical device distributor and ensures your patients get reliable, easy-to-use cellular devices that transmit data automatically.
Potential for new revenue
Now for the best part: how RPM makes you money. RPM isn't just a tool for better patient care; it's a powerful way to generate a new, recurring revenue stream. Medicare and many private payers have specific CPT codes that allow you to bill for the time spent setting up patients, monitoring their data, and communicating with them each month. This creates a predictable source of income that can significantly strengthen your practice's financial health. By leveraging an RPM partner to manage the daily monitoring and documentation, you can capture this revenue without adding a significant workload for your staff, turning patient data into a valuable asset for both care and compensation.
Gains in operational efficiency
Beyond direct reimbursement, RPM delivers a strong return by making your practice more efficient. By automating the collection of daily health data, you reduce the time your staff spends on manual follow-up calls and data entry. The system flags patients whose readings are out of range, allowing your team to focus their attention where it's needed most. This proactive approach helps you intervene earlier, potentially reducing emergency room visits and hospitalizations. It also streamlines how you go about managing chronic conditions, leading to fewer unnecessary office visits and a more manageable workload for your clinical team, which is a huge win for preventing staff burnout.
How to choose the right RPM company for your practice
Choosing a RPM partner is a big decision that will impact your staff, your patients, and your bottom line. With so many options available, it’s important to look beyond the sales pitch and find a company that truly aligns with your practice’s goals. Think of it as hiring a new team member—you want someone reliable, efficient, and easy to work with. The right partner won’t just sell you devices; they’ll provide the technology, support, and expertise needed to build a successful and sustainable program from the ground up. This means finding a company that understands the unique needs of a practice like yours and is committed to helping you achieve better patient outcomes and create a new, recurring revenue stream. Here’s a step-by-step guide to help you find the perfect fit.
Assess your practice's needs
Before you even start looking at vendors, take some time to look inward. What are you hoping to achieve with an RPM program? Your answer will shape your entire selection process. Consider your patient population—are they generally tech-savvy, or will they need simple, out-of-the-box devices? Think about your staff’s current workload. Do you need a partner that handles everything from patient enrollment to billing, or do you have the internal capacity to manage some of these tasks? Understanding the specific challenges of your practice will help you identify which features are must-haves and which are just nice-to-haves, ensuring you choose a solution that creates a sustainable, successful program.
Evaluate the technology
The right technology should make your life easier, not more complicated. When evaluating RPM solutions, focus on usability for both your patients and your clinical team. For patients, look for cellular devices that don't require complicated setup with Bluetooth or Wi-Fi. The easier the device is to use, the more likely your patients will stick with the program. For your staff, the software platform should be intuitive, presenting patient data in a clear, actionable format. A clunky interface or confusing reports will only add to their administrative burden. The goal is to find a RPM system that works seamlessly in the background, empowering you to focus on patient care.
Review patient support options
Technology is only one piece of the puzzle. Consistent patient engagement is what makes an RPM program truly effective, and that requires dedicated support. A great RPM partner acts as an extension of your care team, helping with everything from onboarding new patients to providing ongoing encouragement and technical assistance. Find out what a company’s support structure looks like. Do they have a team that will reach out to patients who aren’t taking readings? Will they help educate patients on the importance of the program? This level of support not only improves adherence but also frees up your staff to focus on clinical duties, making services like CCM much more manageable.
Compare pricing models
Understanding the financial side of an RPM program is critical for its long-term success. Ask for a complete breakdown of all potential costs, including any one-time setup fees, monthly per-patient charges, and device costs. Some companies lease devices, while others require you to purchase them upfront. A transparent pricing model with no hidden fees is a must. More importantly, a good partner will help you understand the path to profitability. They should be able to clearly explain how their services align with reimbursement codes to ensure your program generates a positive return on investment and remains financially sustainable for your practice.
Check for easy integration
To get the most out of your RPM data, it needs to live where you do your work—in your EMR. A solution that doesn’t integrate with your existing systems creates data silos and forces your staff into the time-consuming, error-prone task of manual data entry. This completely defeats the purpose of using technology to create efficiencies. Ask potential partners about their integration capabilities. Do they offer a seamless, bidirectional integration with your specific EMR? A smooth EMR integration ensures that patient data flows directly into their chart, making it a natural part of your clinical workflow rather than an extra administrative step.
Verify security and compliance
When you’re dealing with patient health information, security is non-negotiable. Any RPM company you consider must be fully HIPAA-compliant and have robust security measures in place to protect sensitive data. Don’t be afraid to ask for the details. Inquire about their data encryption methods, both for data in transit from the device and at rest on their servers. Ask them to provide documentation of their HIPAA compliance and security protocols. Partnering with a company that prioritizes security not only protects your practice from potential breaches and legal issues but also builds trust with your patients. You can always review HIPAA basics to ensure you're asking the right questions.
Set up your RPM program for success
Choosing the right RPM company is a huge first step, but the real work begins once you’ve signed on. A successful RPM program doesn’t just happen—it’s built through careful planning and thoughtful execution. The best technology in the world won't make a difference if it doesn't fit into your practice's daily life or if your patients don't use it.
The key is to think of RPM not as a separate, add-on service, but as an integral part of how you deliver care. This means preparing your team, creating a clear plan for bringing patients on board, and making sure the technology works for you, not against you. By focusing on a smooth rollout and continuous improvement, you can build a program that truly supports your patients, empowers your staff, and strengthens your practice's financial health. The following steps will guide you through launching an RPM program that lasts.
Plan your program and train your staff
Before you enroll a single patient, it’s essential to have a solid plan. Start by defining what success looks like for your practice. Are you aiming to reduce hospital readmissions for heart failure patients? Or maybe you want to help your diabetic patients achieve better glycemic control? Setting clear goals will help you focus your efforts. From there, map out the new workflow and assign roles. Who will be responsible for monitoring alerts? Who will reach out to patients?
Proper training is the bridge between your plan and a successful launch. Your team needs to feel confident using the new platform and understand how it fits into their daily responsibilities. A good RPM partner will provide comprehensive training to ensure everyone is comfortable and ready to go from day one.
Create a patient enrollment strategy
Your RPM program is only as effective as the number of patients who participate. A strong enrollment strategy starts with identifying which patients are eligible and would benefit most from the service. Once you have your list, the next step is education. Patients need to understand what RPM is, how it helps them manage their health from home, and what’s expected of them.
Make the sign-up process as simple as possible. Lengthy forms and complicated instructions can be a major barrier. The best approach is a personal one—a conversation with a trusted provider or staff member can make all the difference. Many practices partner with RPM companies that handle enrollment, freeing up your staff to focus on care.
Integrate RPM into your daily workflow
One of the biggest hurdles to adopting new technology is the fear that it will disrupt your practice’s flow. A well-designed RPM solution should feel like a natural extension of your existing workflow, not another complicated system to manage. The goal is to have patient data sync automatically with your EHR.
This seamless integration means your clinical team can see vital signs and trends directly within the patient’s chart, without having to log in to a separate portal. This saves time, reduces the chance of errors, and makes it easier to incorporate RPM data into clinical decision-making during patient visits. When the technology works quietly in the background, your team can focus on what matters most: the patient.
Monitor your program's performance
Once your program is up and running, you’ll want to know if it’s meeting the goals you set. Regularly monitoring your program's performance is key to its long-term success. Look at metrics like patient adherence—are patients taking their readings consistently? Also, track clinical outcomes. Are you seeing improvements in blood pressure or blood glucose levels?
Your RPM platform should provide clear, easy-to-understand reports that give you this insight. Beyond clinical data, keep an eye on your financial return and staff efficiency. These metrics will help you demonstrate the value of the program and identify any areas that need adjustment to ensure you’re getting the most out of your investment.
Keep patient data secure
In healthcare, trust is everything. Patients are sharing their most sensitive health information with you, and they trust you to protect it. That’s why data security is a non-negotiable part of any RPM program. Your chosen solution must be fully HIPAA-compliant, with robust security measures in place to safeguard protected health information (PHI).
This includes using encryption for all data, both when it's being transmitted from a patient's device and when it's stored. A reputable RPM partner will have stringent security protocols built into their platform, giving you and your patients peace of mind. During a Transitional Care Management period, for example, secure data flow is especially critical to ensure continuity and privacy.
Most of the hurdles practices face fall into a few key areas: keeping patients on board, getting new technology to play nicely with your existing systems, making sense of all the new data, and making sure the program works for your staff and your budget.
Overcome common RPM challenges
Adopting an RPM program is a fantastic step toward modernizing your practice and improving patient outcomes. But like any new initiative, it can come with a few speed bumps. The good news is that with the right strategy and partner, these challenges are entirely manageable. Thinking through potential issues ahead of time helps you choose a solution that fits your practice like a glove and sets you up for long-term success.
Most of the hurdles practices face fall into a few key areas: keeping patients on board, getting new technology to play nicely with your existing systems, making sense of all the new data, and making sure the program works for your staff and your budget. Let’s walk through each of these common challenges and talk about practical ways to solve them.
Keeping patients engaged and adherent
One of the biggest questions practices have is, "Will my patients actually use this?" It's a valid concern, especially for older patients or those who aren't comfortable with technology. If a patient finds their monitoring device confusing or forgets to take readings, the program can't deliver results.
The key is to make participation as simple and supportive as possible. This starts with a thoughtful onboarding process that walks patients through how to use their devices. It also means having a dedicated person they can call with questions. Many of the top RPM companies, including 1bios, provide staff to handle patient enrollment, training, and ongoing support. This takes the pressure off your team and addresses the common challenges of RPM before they start.
Integrating new technology smoothly
Your practice already has a workflow and an EMR system you rely on. The last thing you need is a clunky new platform that disrupts everything. A successful RPM program should feel like a natural extension of the care you already provide, not an extra burden. Poor integration can lead to duplicate data entry, frustrated staff, and a system that creates more problems than it solves.
To avoid this, look for an RPM solution built for seamless EMR integration. The goal is to have patient data flow directly and securely into their chart where you can see it. Before committing to a partner, ask for a demo of their platform and inquire about their integration process. The best solutions are designed to be easy to integrate and adopt, with a dedicated support team to manage the setup.
Managing patient data effectively
An RPM program can generate a steady stream of patient data, which is great—but it can also be overwhelming. Sifting through endless readings to find what’s clinically significant is not a good use of your time. Without a system to organize and prioritize this information, you risk missing critical alerts or spending too much time on data review.
Your RPM platform should do the heavy lifting for you. Look for a solution with a clean, intuitive dashboard that flags abnormal readings and highlights trends. This ensures a seamless data flow from the patient's home to their health record, turning raw numbers into actionable insights. Customizable alerts allow you to set specific thresholds for each patient, so you’re only notified when your attention is truly needed.
Getting your staff on board
Your team is essential to the success of any new program. If they see RPM as just another task on their already-full plate, it will be difficult to get the program off the ground. Staff may feel they don't have the time to monitor patients or lack the training to confidently use the new system and data.
The best way to ensure buy-in is to choose a solution that minimizes staff workload. Some RPM companies provide their own clinical teams to monitor patient readings, handle alerts, and engage with patients, offloading the day-to-day work from your practice. This allows your staff to focus on in-office patients while still having access to all the RPM data. When you do need your team to interpret RPM data, make sure your partner provides thorough training and ongoing support.
Staying on budget
Implementing an RPM program is an investment, and you need to be confident that it will pay off. Between device costs, platform fees, and staff time, it’s important to have a clear picture of the total expense. The financial viability of your program also depends on getting properly reimbursed for the services you provide.
Look for an RPM partner with transparent, straightforward pricing. They should be able to provide a clear ROI analysis based on your patient population and typical reimbursement rates. A good partner will also act as your billing expert, ensuring you’re using the right CPT codes and have the documentation needed to pass any audit. This support helps cover the costs of the program and turns it into a reliable new revenue stream for your practice.
As the technology becomes more intelligent and seamless, it will unlock even more powerful ways to deliver high-quality care outside the clinic walls, making your practice more effective and scalable.
The future of RPM
RPM is quickly moving beyond simple data collection and becoming a cornerstone of modern chronic care. The technology is evolving from a reactive tool that flags concerning vitals to a proactive system that helps you anticipate patient needs and streamline your practice's workflow. This shift is driven by smarter technology, broader integration with other virtual care services, and a growing focus on preventative medicine. For practices, this means more opportunities to improve patient outcomes, increase efficiency, and build a more resilient revenue stream.
The future of RPM is about creating a more connected and continuous care experience. Instead of relying on periodic in-office visits, you can gain a constant, real-time understanding of your patients' health between appointments. This allows your team to intervene earlier, provide more personalized guidance, and empower patients to take a more active role in managing their conditions. As the technology becomes more intelligent and seamless, it will unlock even more powerful ways to deliver high-quality care outside the clinic walls, making your practice more effective and scalable.
The next generation of RPM companies will be defined by how well they balance innovation with compliance. 1bios is already leading that shift, embedding AI throughout the monitoring, documentation, and billing process to give practices a scalable, audit-ready foundation for the future of virtual care.
The growing role of AI and machine learning
AI is making RPM systems significantly smarter and more efficient. Instead of just alerting your staff to a high blood pressure reading, AI can analyze trends over time to predict which patients are at the highest risk for an adverse event. This predictive capability helps your clinical team prioritize outreach and focus their attention where it’s needed most. AI also enhances the patient experience by personalizing communication. For instance, an RPM platform can automatically send educational videos or tailored health tips based on a patient's specific data, helping them better understand and manage their health. This transforms RPM from a monitoring tool into a dynamic patient engagement platform.
Deeper integration with virtual care
RPM no longer operates in a silo. It is becoming deeply integrated with other virtual care services like CCM and telehealth. This creates a unified system for managing patients with complex needs. For example, an alert from an RPM device can trigger a telehealth visit, and the time spent reviewing data can count toward CCM billing. This holistic approach provides a more complete picture of a patient's health and ensures they receive continuous, coordinated care. As private payors continue to expand coverage and implement new RPM policies, this integrated model will become even more critical for practices looking to maximize both clinical impact and revenue.
Better tools for population health
The massive growth in RPM adoption provides an incredible opportunity for population health management. The utilization of remote monitoring has skyrocketed, generating a wealth of data that can offer insights into your entire patient panel. By aggregating and analyzing this data, you can identify trends, spot at-risk groups, and implement targeted interventions across your practice. For example, you might notice that a specific group of diabetic patients consistently has high glucose readings in the morning. This insight allows you to proactively reach out with educational resources or schedule follow-up appointments, improving outcomes on a larger scale and using your clinical resources more effectively.
What new technologies are on the horizon?
The next wave of RPM technology will focus on making data collection even more seamless and comprehensive. We're seeing a rise in medical-grade wearables—like smartwatches, rings, and skin patches—that can passively monitor vitals without requiring any action from the patient. These devices can track a wider range of metrics, including sleep quality, activity levels, and even stress indicators, providing a more holistic view of a patient's well-being. The outlook for connected medical devices suggests a future where continuous, multi-faceted data streams give clinicians a richer, more detailed understanding of patient health, further reducing the burden on both patients and staff.
Related articles
- Turnkey Remote Patient Monitoring (RPM)
- 3 Reasons Remote Patient Monitoring (RPM) is Great for your Patients
- 5 Ways New Technologies are Making Remote Patient Monitoring (RPM) Easy
- Remote Patient Monitoring (RPM) Monitoring Team: Insource vs. Outsource
Frequently asked questions
My staff is already stretched thin. How much extra work does an RPM program really add?
This is one of the most important questions to ask, and the answer depends entirely on the partner you choose. If you opt for a technology-only platform, your team will be responsible for all the daily monitoring, patient communication, and troubleshooting. However, a full-service partner provides their own clinical team to handle these tasks for you. This approach is designed to offload work from your staff, not add to it, allowing you to gain the clinical and financial benefits of RPM without the operational burden.
Will my patients, especially older ones, actually be able to use the technology?
It’s a common concern, but modern RPM is designed for simplicity. The best programs use cellular-enabled devices that work right out of the box, with no need for Wi-Fi, smartphones, or complicated setup. A great partner also takes responsibility for patient success by handling the initial training, providing clear instructions, and offering ongoing support. This ensures your patients feel confident and your staff isn't stuck playing tech support.
How do I know if the revenue from RPM will be worth the cost?
Think of RPM as an investment that pays for itself. The costs, such as monthly service fees, are structured to be more than covered by the reimbursements from Medicare and many private insurance plans. A transparent partner will provide a clear financial projection based on your patient population. They should also offer billing support to make sure you have the right documentation to capture all the revenue you’ve earned, turning the program into a sustainable and profitable part of your practice.
What’s the real difference between a full-service RPM company and a tech-only platform?
A tech-only platform provides the software and devices, but your team is responsible for running the entire program—from enrolling patients to monitoring daily data. A full-service partner, on the other hand, acts as an extension of your practice. They provide not only the technology but also the trained clinical staff to manage the day-to-day operations. It’s the difference between buying a tool and hiring an expert team to do the work for you.
How long does it take to get an RPM program started in my practice?
Getting started is much faster and simpler than you might think. With a dedicated partner, you can be up and running in just a few weeks. The right company will manage the entire implementation process, including the technical setup, integrating with your EMR, and training your staff. They do the heavy lifting so you can focus on identifying the right patients and preparing for a smooth launch.